Cardiac & Heart Attack
About Us
Aloha and welcome to our hospital’s dedicated STEMI (ST-Elevation Myocardial Infarction) team, where our commitment to excellence in cardiac care is reflected in our remarkable statistics and unwavering dedication to saving lives. Over the past three years, our team has consistently demonstrated exceptional performance and a commitment to ensuring timely and effective interventions for patients experiencing acute cardiac events.
In 2020, our team successfully managed 54 cases of STEMI, with an additional 16 patients transferred to our facility for specialized care. This marked the beginning of our journey to provide top-notch cardiac services to our community.
In the subsequent year, 2021, our team continued to rise to the challenge, handling 42 cases of STEMI within our hospital and an impressive 28 transferred cases. This increase in transferred cases demonstrates the trust placed in our team by neighboring healthcare facilities seeking our expertise in managing critical cardiac emergencies.
Building on our achievements, 2022 proved to be a banner year for our STEMI team, as we efficiently addressed 58 cases of STEMI within our hospital and extended our expertise to 31 transferred cases. This growth showcases our team’s continual commitment to advancing and improving our capabilities in providing life-saving interventions.
As we move forward, our STEMI team remains dedicated to staying at the forefront of cardiac care, embracing innovation, and delivering compassionate, patient-centered services. We take pride in our accomplishments and look forward to furthering our impact on cardiac health in the coming years. Together, we stand united in our mission to provide the highest standard of care for every patient who entrusts us with their cardiovascular well-being.
Cardiac & Heart Attack
Learn More
What is a Heart Attack (STEMI)?
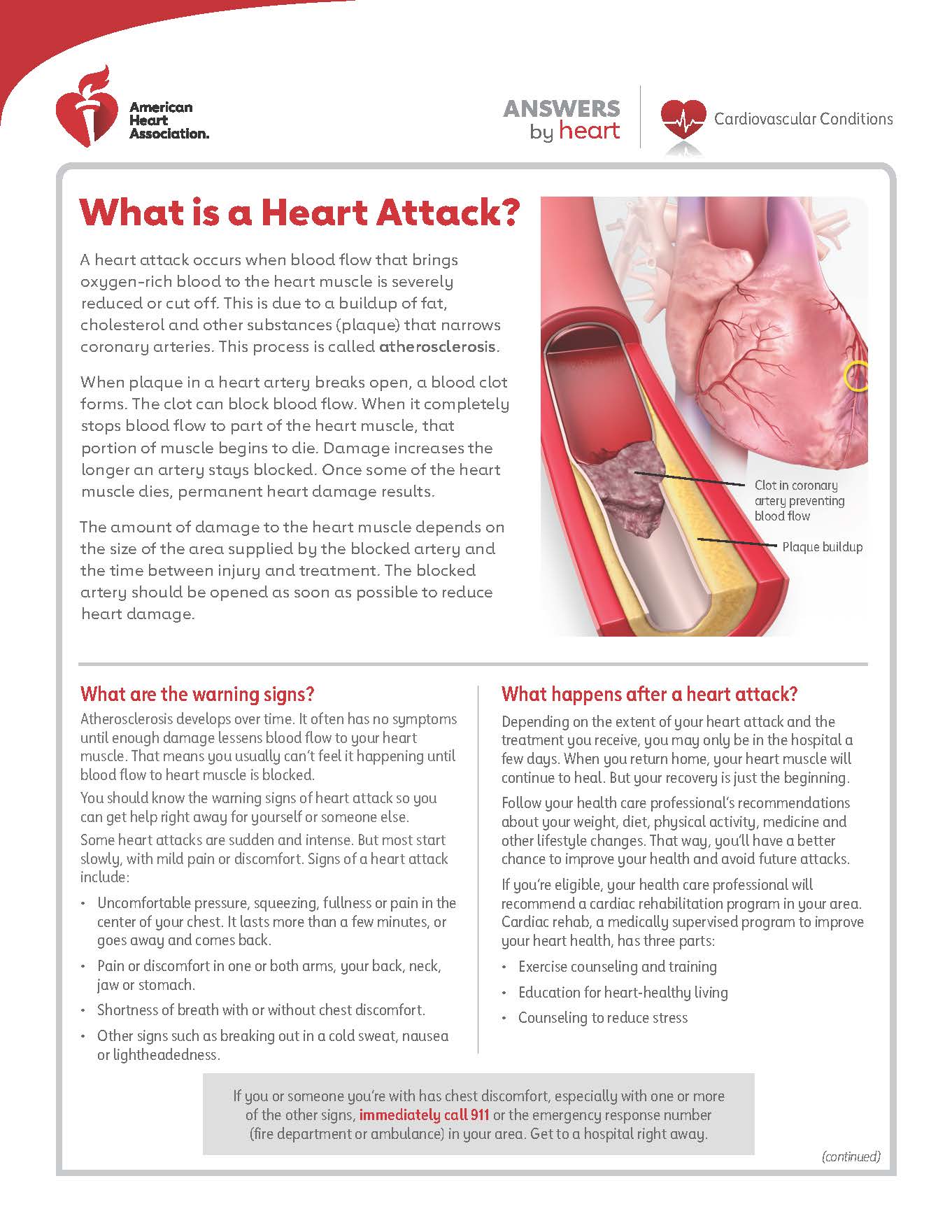
A heart attack occurs when the blood flow that brings oxygen-rich blood to the heart muscle is severely reduced or cut off. This is due to a buildup of fat, cholesterol, and other substances (plaque) that narrows coronary arteries. This process is called atherosclerosis.
When plaque in a heart artery breaks open, a blood clot forms. The clot can block blood flow. When it completely stops blood flow to part of the heart muscle, that portion of muscle begins to die. Damage to the heart muscle increases the longer an artery stays blocked. Once some of the heart muscle dies, permanent heart damage results.
The amount of damage to the heart muscle depends on the size of the area supplied by the blocked artery and the time between injury and treatment. The blocked artery should be opened as soon as possible to reduce heart damage.
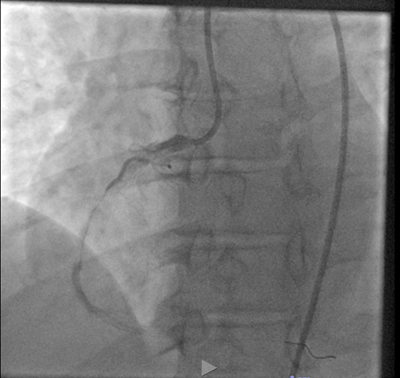
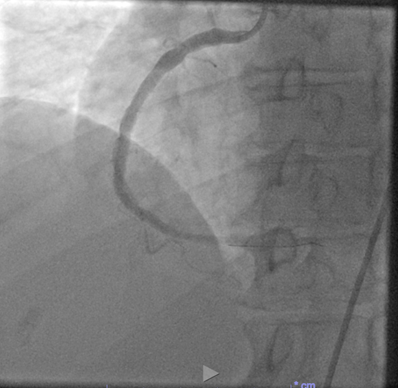
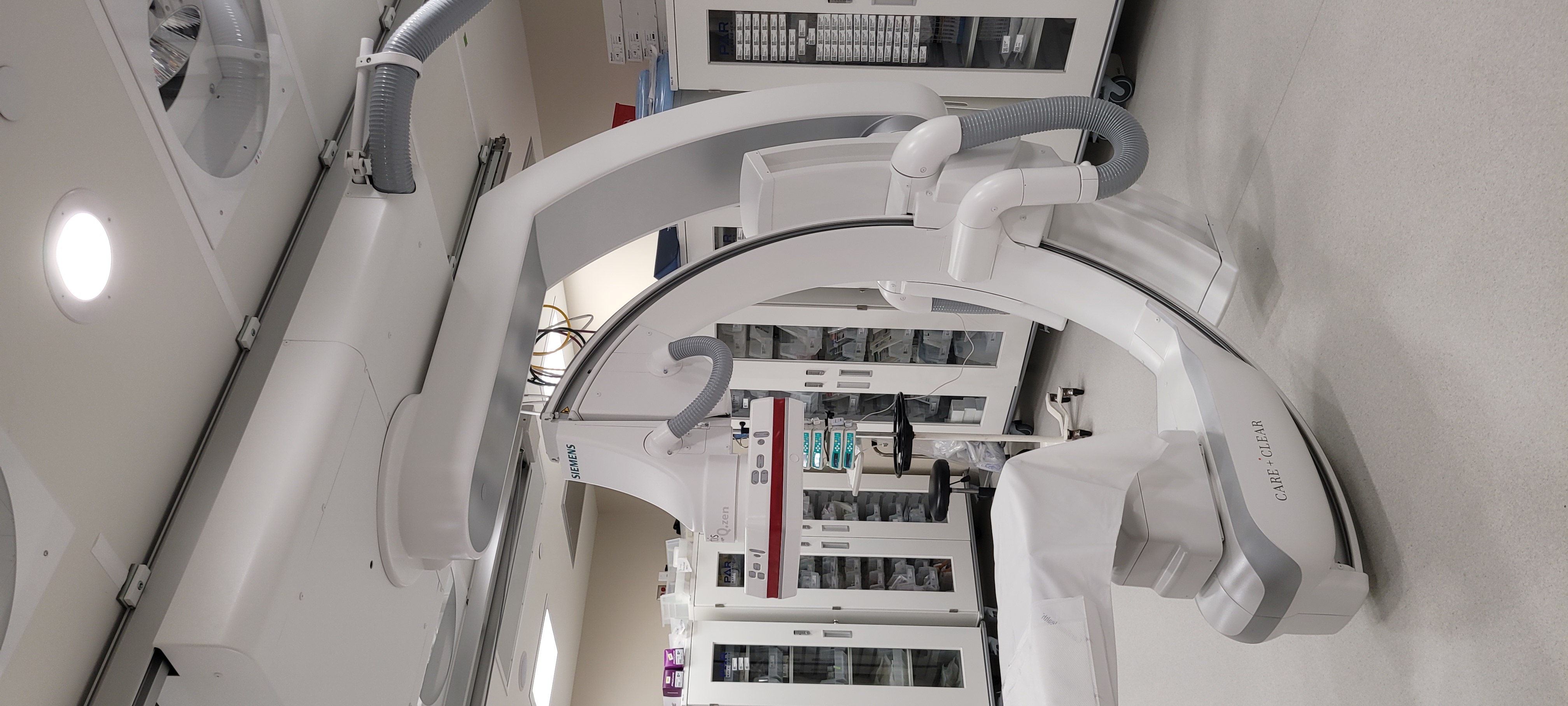
At Hilo Medical Center, we treat our STEMI patients with a percutaneous coronary intervention (PCI) in our cardiac cath lab.
What is a NSTEMI?
- • When the coronary artery is partially blocked is an “NSTEMI” or a non-ST-elevation myocardial infarction.

Treatment for a Heart Attack (STEMI)
What is cardiac catheterization?
- • Cardiac catheterization (cardiac cath or heart cath) uses a very small tube called a catheter to insert either in the radial artery or the femoral artery to examine how well your heart is working. It is used to diagnose some heart problems.
- • A catheter is used to diagnose and treat heart disease. Catheters are very small tubes (similar to IVs) that healthcare providers put through your blood vessels.
What are the risks of cardiac catheterization?
- • Bruises where the catheter had been inserted (puncture site).
- • Bleeding at the puncture site.
- • Reaction to the contrast dye.
- • Infection.
Some other risks include:
- • Stroke
- • Heart Attack
- • Abnormal heart rhythm
- • Blood clots to other parts of the body
- • Damage to a blood vessel or heart from the catheter
- • Heart attack
- • Bleeding
- • Death
What happens during cardiac catheterization?
A doctor with special training performs the procedure with a team of nurses and technicians. The procedure is done in a cardiac catheterization (cath lab) at a hospital or medical clinic.
- • Before the cath procedure, a nurse will put an IV (intravenous) line into a vein in your arm so you can get medicine (sedative) to help you relax, but you’ll be awake and able to follow instructions during the procedure.
- • The nurse will clean and shave the area where the doctor will be working. This is usually in the forearm or groin area.
- • The doctor will make a needle puncture through your skin and into a large blood vessel. A small straw-sized tube (called a sheath) will be inserted into the vessel. The doctor will gently guide a catheter (a long, thin tube) into your vessel through the sheath. A video screen will show the position of the catheter as it is threaded through the major blood vessels and to the heart. You may feel some pressure in your arm or groin, but you shouldn’t feel any pain.
- • Various instruments may be placed at the tip of the catheter. They include instruments to measure the pressure of blood in each heart chamber and in blood vessels connected to the heart, view the interior of blood vessels, take blood samples from different parts of the heart, or remove a tissue sample from inside the heart.
- • When a catheter is used to inject a dye that can be seen on X-rays, the procedure is called angiography.
- • When a catheter is used to clear a narrowed or blocked artery, the procedure is called angioplasty or a percutaneous coronary intervention.
- • When a catheter is used to widen a narrowed heart valve opening, the procedure is called valvuloplasty.
- • The doctor will remove the catheters and the sheath. Your nurse will put pressure on the site to prevent bleeding. Sometimes a special closure device is used.
How do I know if my heart is permanently damaged?
When a heart attack (STEMI) occurs, the heart muscle that has lost oxygen and blood supply begins to result in damage. The amount of damage to the heart muscle depends on the size of the area supplied by the blocked artery and the time between injury and intervention.
Heart muscle damaged by a heart attack heals by forming scar tissue. It usually takes several weeks for your heart muscle to heal. The length of time to recover depends on your injury’s extent and comorbidities.
Even if part of your heart is damaged, the rest of the heart continues to work. Due to the damage in your heart, it may be weakened and unable to pump as much blood as usual.
Further heart damage can be prevented with lifestyle changes.
How long will it take to recover from my heart attack?
Talk to your healthcare professional about your recovery time. Heart attacks can have longer or shorter recoveries and complications. Recovery depends on the size and location of the damage and how soon treatment of your heart attack occurred.
After a heart attack (STEMI), the heart muscle may have damaged areas, and scar tissue may form. When scar tissue forms, it prevents the heart from pumping and contracting healthy cardiac muscle. As a result, the extent of damage to the heart muscle can affect how well the heart pumps blood throughout the body.
How much pumping function is lost depends on the size and location of the scar tissue. Most heart attack survivors have some degree of coronary artery disease (CAD) and must make significant lifestyle changes and possibly take medication(s) to prevent a future heart attack.
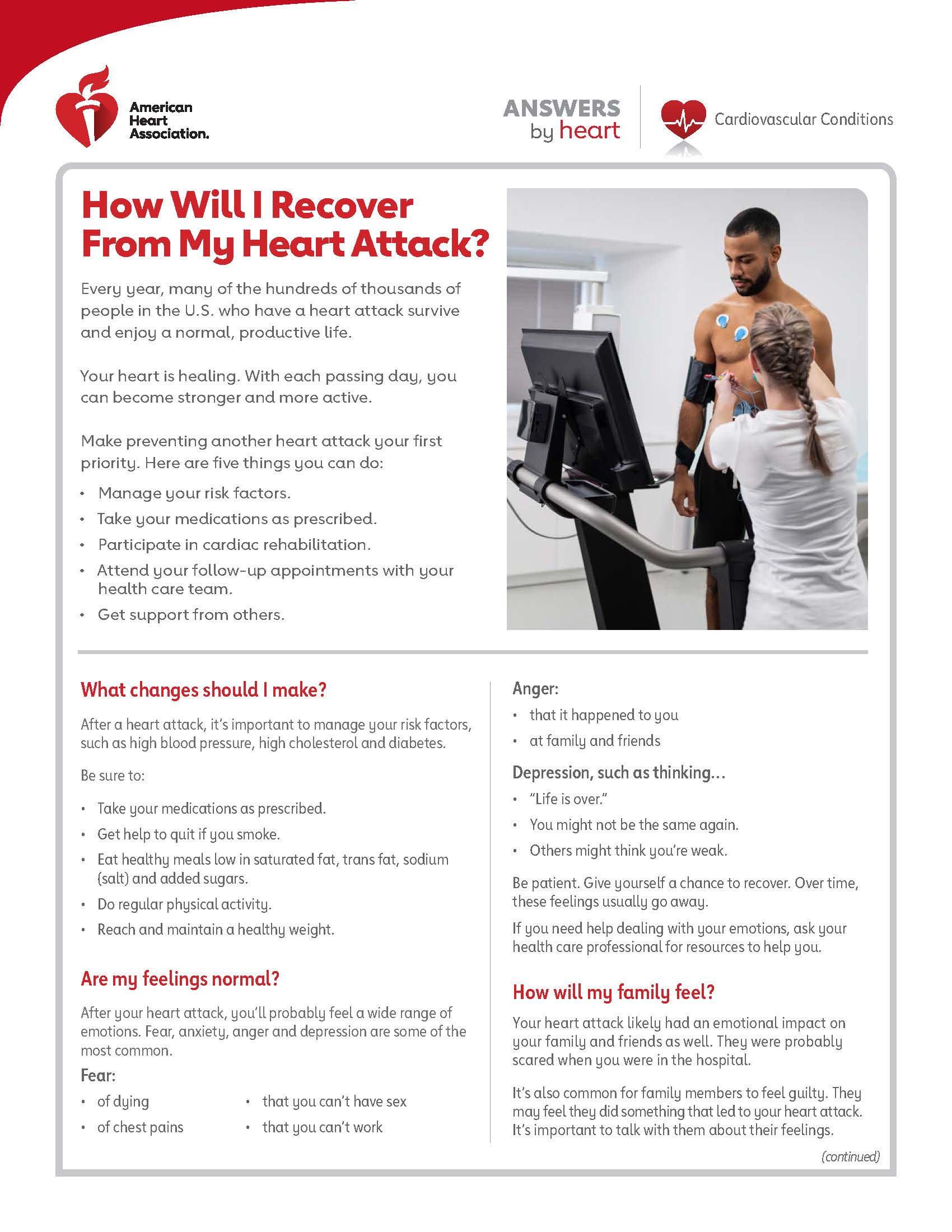
Cardiac Rehabilitation
Our Cardiac Rehab Team provides a medically supervised program designed to improve your heart health after heart problems or surgery.
You may be eligible for this service if you have had a:
- • Heart attack in the last 12 months
- • Heart condition such as stable angina or heart failure
- • Heart procedure(s) or surgery such as:
- ◦ Coronary artery bypass graft (CABG) surgery
- ◦ Angioplasty and stenting
- ◦ Heart valve repair or replacement
Cardiac Rehab is delivered in a group setting with other heart patients with heart related conditions. With the oversight of healthcare professionals, you receive monitored exercise to strengthen the heart and to improve cardiac endurance. Information and education is provided during each session to assist you in managing modifiable risk factors such as: diabetes, hypertension, high cholesterol.
How can I reduce my risk for a heart attack?
Even if you have heart disease, you can do a lot to improve your heart health. Work with your healthcare team to reduce your risk. Some ways to reduce the chances of having a heart attack are:
• Don’t smoke or vape and avoid secondhand smoke.
• If you don’t drink, don’t start.
• Visit your provider for regular checkups
• Get at least 150 minutes of moderate-intensity physical activity a week.
• Reach and maintain a healthy weight.
• Control your blood sugar if you have diabetes.
• Get at least seven hours of sleep every nigh
• Manage your stress.
Is all chest pain a heart attack?
No, not all chest pain is a heart attack. If you are experiencing chest pain or discomfort, you should see a healthcare professional immediately by calling 9-1-1. One common type of chest pain is called angina. Angina is a recurring chest discomfort that usually lasts for a few minutes. Angina occurs when your heart muscle doesn’t get the blood supply and oxygen it needs and signals that you’re at higher risk of a heart attack.
The difference between angina and a heart attack is that angina attacks does not permanently damage the heart muscle.
• Don’t do illegal drugs such as
- ◦ Methamphetamine- can increase heart rate and blood pressure and reduce your heart’s overall function.
- ◦ Cocaine- can cause high blood pressure, thickening of your cardiac arteries, and thickness of the heart’s left ventricle.
• Manage your risk factors such as hypertension, diabetes, smoking, and high cholesterol.
• Take your prescribed medication(s) and don’t stop unless talking to your health care provider.
• Treat your high blood pressure, if you have it, according to your health care professional’s recommendations.
• Eat a heart-healthy diet that’s low in saturated and trans fats, sodium (salt) and added sugars.
• Drink in moderation.
- ◦ Drinking too much alcohol can raise your triglycerides.
- ◦ Excessive drinking can lead to high blood pressure, cardiomyopathy and arrhythmias.
Cardiac Medications
- • Anticoagulant: Used to treat certain blood vessel, heart and lung conditions.
- • Antiplatelet agent: Keeps blood clots from forming by preventing blood platelets from sticking together.
- • Angiotensin-converting enzyme (ACE) inhibitor: Expands blood vessels and decreases resistance by lowering levels of angiotensin II. Allows blood to flow more easily and makes the heart’s work easier or more efficient.
- • Angiotensin II receptor blocker: Rather than lowering levels of angiotensin II (as ACE inhibitors do) angiotensin II receptor blockers prevent this chemical from having any effects on the heart and blood vessels. This keeps blood pressure from rising.
- • Beta blocker: Decreases the heart rate and cardiac output, which lowers blood pressure and makes the heart beat more slowly, with less force.
- • Combined alpha and beta blocker: Combined alpha and beta blockers are used as an IV drip for those patients experiencing a hypertensive crisis. They may be prescribed for outpatient high blood pressure use if the patient is at risk for heart failure.
- • Calcium channel blocker: Interrupts the movement of calcium into the cells of the heart and blood vessels. May decrease the heart’s pumping strength and relax the blood vessels.
- • Cholesterol-lowering medications: Various medications can lower blood cholesterol levels, but statins are the best first course of action. When statins prove ineffective, or if a patient experiences serious side effects from statin therapy, other drugs may be recommended.
- • Diuretics: Cause the body to rid itself of excess fluids and sodium through urination. Help to relieve the heart’s workload. Diuretics also decrease the buildup of fluid in the lungs and other parts of the body, such as the ankles and legs. Different diuretics remove fluid at varied rates and through different methods.